All published articles of this journal are available on ScienceDirect.
Individual and Household Practices for Mitigating and Preventing Indoor Air Pollution Among Health Professional Students: A Self-Report Study
Abstract
Introduction
Indoor air pollution is a significant environmental issue linked to a range of short- and long-term health consequences, including respiratory disorders, cancer, and premature death. It often results from common household activities, yet practices to mitigate its impact are frequently neglected. This study aimed to explore individual and household-level practices for indoor air pollution mitigation and prevention and its associated factors among health professional students.
Methods
A descriptive survey was conducted among 388 health professional students enrolled in undergraduate nursing and dental programs, recruited using consecutive sampling. Sociodemographic profiles and a five-point Likert scale were used to collect data on participants' backgrounds and their individual and household-level practices for mitigating and preventing indoor air pollution. Both descriptive and inferential statistics were used for the data analysis.
Results
Most of the undergraduates, 71.1%, were engaged in high levels of IAP mitigation and prevention practices. Dental undergraduates practiced significantly better than nursing undergraduates in terms of keeping windows open for natural ventilation, washing bedding, pillows, and curtains regularly, and cleaning the top of the ceiling fan blades. However, they were also more likely to allow people to wear outdoor shoes inside the house. Gender and marital status were significantly associated with IAP mitigation strategies (p < 0.05). Limited exposure to workshops or seminars on IAP (86.1% of participants) may explain moderate adherence levels.
Discussion
The results underscore the importance of integrating environmental health awareness into health professional training, as even future healthcare providers demonstrate inconsistent adherence to key indoor air pollution (IAP) prevention practices. These findings align with existing research indicating low public engagement with IAP mitigation despite well-documented health risks, highlighting the need for targeted education. However, the study is limited by its reliance on self-reported data and a single-institution sample, which may affect the generalizability and accuracy of the results.
Conclusion
Although health professional students displayed moderate to high self-care behaviors, gaps in specific practices and demographic disparities highlight the need for targeted educational interventions. Integrating environmental health education into health professional curricula could enhance awareness and practice levels.
1. BACKGROUND
Indoor air pollution is a significant public health issue impacting millions of people globally. (Afolabi et al. 2016; Tran et al. 2020). The World Health Organization (WHO) has identified air pollution as “the world's largest single environmental health risk.” It is estimated to contribute to 4% of deaths globally, amounting to approximately 3.8 million deaths, with a significant proportion being premature deaths occurring in developing countries (Wang et al. 2016; Tran et al. 2020). Globally, more than 1 billion people, approximately 8% of the world’s population, breathe polluted air, as reported by the United Nations Environment Program (UNEP) (Zeng et al. 2017; Ratnasari et al. 2024). Furthermore, poor air quality is expected to be exacerbated by growing urbanization, industry, and climate change in the coming decades (Silva et al. 2017; Deswal et al. 2020).
While outdoor air pollution often garners more attention, the problem of indoor air quality is often neglected. Unlike indoor air pollution, driven mainly by industrial emissions, transportation (especially vehicle exhaust), and power generation, contributing to higher levels of nitrogen oxides (NOx), sulfur oxides (SOx), and coarse particulate matter (PM10), indoor air pollution primarily arises from household activities such as cooking, heating, cleaning, and the use of consumer products. These activities release pollutants like volatile organic compounds (VOCs), carbon monoxide (CO), and fine particulate matter (PM2.5) (Milojević et al., 2024). As per recent reports, poor indoor air quality is a critical yet frequently overlooked health concern with serious implications. It is linked to a variety of health conditions, including but not limited to low birth weight, fetal loss, respiratory, cardiovascular, neurological, ocular, and oncologic conditions, sick-building syndrome, and even premature deaths (Steinle et al. 2015; Cascio and Long 2018). Given that the levels of indoor pollutants are two to hundred times higher than the outdoor indoor air pollution (IAP), understanding and mitigating IAP is essential (Saraga et al. 2023).
Improving air quality is one of the key agendas of the United Arab Emirates (UAE) National Vision, as nearly 6.5 million people die from exposure to indoor and outdoor air pollution every year in the country. The country witnesses the negative impact of air pollution not only in health but extend in other economic and social aspects as well (Akasha et al. 2024). Rapid urbanization, industrialization, unique cultural and climatic conditions, and widespread use of air conditioning systems, necessitated by the region’s hot desert climate, fueled by the accelerated transitions that have occurred in the last five decades, have made indoor air pollution a pressing concern in the United Arab Emirates (Akasha et al. 2024; Alahmad et al. 2024).
Preventing and mitigating indoor air pollution involves controlling potential sources and raising awareness of individual and household-level practices against IAP (Nair et al. 2022; Jung and Abdelaziz Mahmoud 2023; Saraga et al. 2023) These encompassing a range of practices, including but not limited to increasing ventilation, avoiding indoor tobacco use, identifying and eliminating pollution sources, use of air purification filters, control of humidity and temperature, and regular maintenance of HVAC systems (Nair et al. 2022; Jung and Abdelaziz Mahmoud 2023; Ravi et al. 2024b; Ravi et al. 2024a; Ridolo et al. 2024; Ravi et al. 2025). Using renewable energy sources such as geothermal and solar energy for heating can reduce the emissions from traditional heating systems, as these can cause both indoor and outdoor pollution. (Skrúcaný et al. 2018).
Given its significance, promoting environmental literacy is crucial to effectively addressing health and well-being (Lindsey et al., 2021; Ravi and Mohamed, 2022; Gipson et al., 2024). Health professionals play a critical role in advancing public health and safety in this regard. They can advocate public policies that aim to prevent or reduce the risks of air pollution to human health (Cammalleri et al. 2020; Ravi et al. 2024b; Ravi et al. 2024a; Ravi et al. 2025). Therefore, awareness and practices of healthcare professionals regarding air pollution are fundamental for implementing effective counselling programs aimed at educating the general population on this critical topic.
However, limited evidence is available on indoor air pollution (IAP), with most research focusing primarily on outdoor air quality and pollution. Few studies have explored indoor air pollutants or quality, but research on this topic remains sparse (Funk et al. 2014; Jung et al. 2022). For health professional students, understanding and implementing self-care practices related to IAP is essential not only for their own well-being but also for setting an example in their future roles as healthcare providers (Ravi and Mohamed, 2022; Browne and Chun Tie, 2024). These students will eventually become leaders in healthcare, expected not only to address health issues but also to advocate for preventive measures within their communities (Cammalleri et al. 2020; Soares et al. 2021; Ravi et al. 2024a; Ravi et al. 2024b). Understanding the practices of future professionals regarding the mitigation and prevention of IAP is crucial for developing educational strategies that promote healthier living environments (Jung et al. 2022; Bozzola et al. 2024). Given the lack of research, this study was undertaken to explore the individual and household-level practices for IAP mitigation and prevention among health professional students. This research is timely, aligning with ongoing efforts to improve environmental health standards and promote sustainable living practices in the UAE.
2. METHODOLOGY
2.1. Study Design & Participants
A descriptive research survey design was used to collect data from 260 nursing and 258 dental undergraduates, totaling 518 participants, selected consecutively from the RAK Medical and Health Sciences University in the United Arab Emirates. Out Of these, 388 undergraduates responded to the questionnaire, constituting a response rate of 74.9%.
All undergraduate nursing and dental students aged above 18 years, enrolled in the academic year 2022-23, and willing to participate were included in the study. No specific exclusion criteria were applied. The sample size was calculated using the Raosoft software, which was estimated to be 235 (http://www.raosoft.com/samplesize.html) (Allen and Barn, 2020; Carlsten et al., 2020). The questionnaire was distributed to all eligible students to increase the generalizability and validity of the findings.
2.2. Data Collection Instruments
Data were collected using a self-developed, structured questionnaire. The questionnaire was developed by the researchers after an extensive review of the literature and consultation with experts (Bakhtari Aghdam et al. 2019; Allen and Barn 2020). The questionnaire demonstrated acceptable content validity (CVI-0.92) and reliability (Cronbach’s α = 0.828). Section one of the questionnaires gathered information regarding the characteristics of the participants, including age, gender, nationality, and program enrolled. Section two collected information regarding individual and household-level practices for indoor air pollution mitigation and prevention related to indoor air pollution using a five-point Likert scale. The final score of practice was calculated by adding up the points obtained for the corresponding questions and categorized as high (score ≥ 80%), moderate (score 50- 80%), and low (score <50%). A pilot study was conducted to ensure feasibility and practicality and to finalize the methods for data analysis. Data collection was carried out in the classroom using Google Forms during their free time after providing details about the purpose and nature of the study.
2.3. Ethical Considerations
The clearance for the study was obtained from the institutional review board of the university where the study was conducted (RAKMHSU-REC-006-2022/23-F-N). Written informed consent was obtained from all participants while ensuring confidentiality and anonymity.
2.4. Data Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 27.0 (IBM, Chicago, IL, USA). Descriptive statistics were presented as frequency, percentages, mean median, interquartile range (IQR), and standard deviation scores, while inferential statistics, such as the Mann-Whitney U test and t-test, were used to assess statistical significance. A p-value of <0.05 was considered statistically significant.
3. RESULTS
3.1. Profile of Participants
Most of them were aged 20 years or below (54.12%), were single (94.8%), female (69.07%), non -Emirati (89.9%), never attended any workshops, enrolled in nursing programs (64.4%), or seminars regarding IAP (86.1%).
3.2. Individual and Household Level Practices for Indoor Air Pollution Mitigation and Prevention
Table 1 shows that mopping, dusting, sweeping, and opening the windows or doors for natural ventilation were performed monthly by the participants. Allowing people to smoke inside homes, allowing people to wear outdoor shoes inside the house, and washing bedding, pillows, and curtains were always practiced. Participants always checked and cleaned or replaced AC filters, along with regular cleaning of the top of the ceiling fan blades.
Table 2 shows that nursing students were more likely to open windows (p = 0.038) and doors (p = 0.013) for natural ventilation, clean ceiling fan blades (p = 0.033), and restrict outdoor shoes inside the house (p = 0.035) compared to Dental participants. Additionally, they reported washing bedding, pillows, and curtains more frequently, with a highly significant difference (p = 0.001). However, other behaviours, such as mopping, dusting, sweeping, checking AC filters, and allowing smoking indoors, showed no statistically significant differences (p > 0.05), indicating similar practices between the two groups.
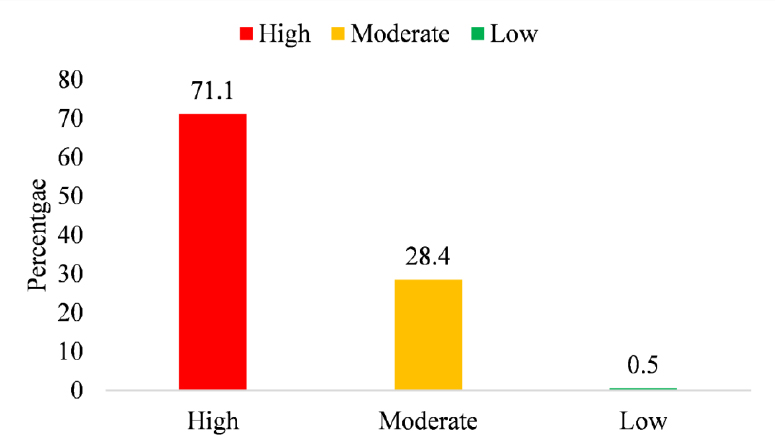
Fig. (1) illustrates the distribution of individual and household level practices for IAP mitigation and prevention among students. The majority, 71.1%, fell into the high level, followed by 28.4% in the moderate level, and only a small fraction, 0.5%) were classified as having low-level practices.
| Self-care behaviors |
Daily n (%) |
Twice in a week n (%) |
Once in a week n (%) |
Once in two weeks n (%) |
Monthly n (%) |
|---|---|---|---|---|---|
| How often do you mop? | 6 (1.5) | 10 (2.6) | 64 (16.5) | 110 (28.4) | 198 (51.0) |
| How often do you dust? | 6 (1.5) | 16 (4.1) | 114 (29.4) | 98 (25.3) | 154 (39.7) |
| How often do you sweep or dust? | 4 (1.0) | 24 (6.2) | 70 (18.0) | 98 (25.3) | 192 (49.5) |
| How often do you open the windows for natural ventilation? | 14 (3.6) | 22 (5.7) | 66 (17.0) | 74 (19.1) | 212 (54.6) |
| How often do you open the doors for natural ventilation? | 20 (5.2) | 22 (5.7) | 80 (20.6) | 82 (21.1) | 184 (47.4) |
|
Never n (%) |
Rarely n (%) |
Sometimes n (%) |
Often n (%) |
Always n (%) |
|
| Do you allow people to smoke inside your home | 0 (0.0) | 0 (0.0) | 58 (14.9) | 52 (13.4) | 278 (71.6) |
| Do you wash your bedding, pillows, and curtains regularly? | 0 (0.0) | 0 (0.0) | 70 (18.0) | 42 (10.8) | 276 (71.1) |
| Do you check and clean or replace AC filters regularly | 0 (0.0) | 0 (0.0) | 104 (26.8) | 46 (11.9) | 238 (61.3) |
| Do you clean the top of your ceiling fan blades | 0 (0.0) | 0 (0.0) | 98 (25.3) | 64 (16.5) | 226 (58.2) |
| Do you allow people to wear outdoor shoes inside the house | 0 (0.0) | 0 (0.0) | 76 (19.6) | 68 (17.5) | 244 (62.9) |
Level of individual and household level practices for mitigation and prevention of IAP among students.
| Variables | Nursing | Dental | Mann Whitney U Value | p-value |
|---|---|---|---|---|
| Self-care behaviors | Median (IQR) | Median (IQR) | - | - |
| How often do you mop? | 5.00 (4.00-5.00) | 4.00 (4.00-5.00) | 15674 | 0.104 |
| How often do you dust? | 4.00 (3.00-5.00) | 4.00 (3.00-5.00) | 16890 | 0.719 |
| How often do you sweep or dust? | 5.00 (3.00-5.00) | 4.00 (4.00-5.00) | 17164 | 0.930 |
| How often do you open the windows for natural ventilation? | 5.00 (3.00-5.00) | 5.00 (4.00-5.00) | 15262 | 0.038* |
| How often do you open the doors for natural ventilation? | 5.00 (3.00-5.00) | 4.00 (3.00-5.00) | 14792 | 0.013* |
| Do you allow people to smoke inside your home | 5.00 (4.00-5.00) | 5.00 (4.00-5.00) | 17030 | 0.793 |
| Do you wash your bedding, pillows, and curtains regularly? | 5.00 (4.00-5.00) | 5.00 (5.00-5.00) | 14552 | 0.001** |
| Do you check and clean or replace AC filters regularly | 5.00 (3.00-5.00) | 5.00 (3.00-5.00) | 16850 | 0.662 |
| Do you clean the top of your ceiling fan blades | 5.00 (4.00-5.00) | 5.00 (3.00-5.00) | 15260 | 0.033* |
| Do you allow people to wear outdoor shoes inside the house | 5.00 (4.00-5.00) | 5.00 (4.00-5.00) | 15330 | 0.035* |
| Variables | N | Mean | SD | Median (IQR) | p- Value |
|---|---|---|---|---|---|
| Age | |||||
| < 20 | 210 | 42.99 | 5.26 | 44 (39-48) | 0.891 |
| ≥ 20 | 178 | 42.45 | 6.51 | 43 (38-48) | |
| Gender | |||||
| Male | 120 | 41.58 | 5.60 | 42 (37-46.75) | 0.002** |
| Female | 268 | 43.26 | 5.91 | 45 (40-48) | |
| Marital Status | |||||
| Unmarried | 368 | 42.59 | 5.84 | 44 (38 – 48) | 0.025* |
| Married | 20 | 45.60 | 5.72 | 48 (41 – 50) | |
| Nationality | |||||
| Emirati | 74 | 43.27 | 7.00 | 46 (37.75-49) | 0.390 |
| Non-Emirati | 314 | 42.62 | 5.69 | 44 (39-47.25) | |
| Program Enrolled | |||||
| Nursing | 250 | 42.74 | 6.13 | 44 (38.75-48) | 0.994 |
| Dental | 138 | 42.74 | 5.38 | 44 (38.75-47) | |
| Symptoms | |||||
| Yes | 142 | 42.69 | 5.73 | 44 (39-48) | 0.783 |
| No | 246 | 42.77 | 6.00 | 44 (38-48) | |
3.3. Association between Practices and Selected Variables
Table 3 illustrates the comparison between the study variables of the participants and their practices related to air pollution. A statistically significant difference (p<0.05) was observed between only two variables, namely gender and marital status, and their practices related to air pollution.
4. DISCUSSION
This study explored individual and household-level practices to mitigate and prevent IAP among 388 undergraduate nursing and dental students at a university in the United Arab Emirates. This cross-sectional study revealed moderate-to-high levels of engagement in individual and household level practices. These findings corroborate those of earlier studies that reported similar levels of engagement among professional health students and the general public (Al-Shidi et al. 2021; Alzayani and Alsabbagh 2022; Meer et al. 2022). The moderate levels of practice reported by participants in this study may stem from insufficient exposure to awareness programs, as indicated by their limited participation in workshops and seminars, suggesting that structured educational interventions may significantly influence the adoption of proactive self-care behaviors (Tuncer 2011; Ahmed et al. 2020; Vasileva et al. 2021). Furthermore, the current study's sample, predominantly female and enrolled in healthcare programs, emphasized that health education and gender-specific traits often foster higher adherence to cleanliness and health-related practices (Kabir et al. 2021; Kligler et al. 2021; Vasileva et al. 2021; Baba et al. 2024)
The findings indicated that students engaged in practices such as mopping, dusting, and sweeping on a monthly basis, while behaviors such as washing bedding and replacing AC filters were performed more consistently. These results align with those of previous studies, which reported that individuals tend to practice routine maintenance behaviors less frequently owing to perceived inconvenience. Individuals with prior education on indoor air quality were notably more consistent with daily cleaning practices, highlighting the importance of awareness campaigns. The predominance of female participants in the current study may explain the higher adherence rates to cleaning behaviors, consistent with gender-specific findings in the literature, where females are often more involved in household tasks (Wang, 2024).
Furthermore, the lack of perceived importance of ventilation aligns with studies showing poor practices despite some level of awareness (Reddy 2016). However, a U.S. study found that nursing students frequently used ventilation (Diaz and Patiño [no date]). In contrast to the findings of this study, participants rarely opened windows or doors and did not support interventions, such as air monitors or smoking bans. Infrequent cleaning also reflects the perceived low importance of air quality. The positive correlation between awareness and behavior suggests that education could effectively promote beneficial practices, as demonstrated by previous interventions. However, the weak correlation highlights the need for multifaceted approaches to maximize the adoption of self-care behaviors. Nursing curricula should emphasize the importance of self-care practices that maintain healthy indoor air quality to enhance students' competencies in identifying and preventing indoor air pollution risks, particularly for vulnerable populations, such as children and individuals with respiratory conditions. Additionally, nurses should model beneficial practices for reducing indoor pollutants in their work settings and advocate institutional and public policies to improve air quality monitoring, building standards, and product regulations (Ravi and Mohamed 2022; Doheny et al. 2023; Ravi et al. 2024a).
Significant associations were observed between gender, marital status, and self-care practices. Females and married individuals exhibited higher engagement levels, consistent with research that linked these variables with heightened environmental responsibility (Wang et al. 2016; Tran et al. 2020; Baby et al. 2024). However, the lack of a relationship with age contrasts findings that reported age as a determinant in adopting health-oriented behaviors. This discrepancy could stem from the homogeneity of age groups in the current sample, limiting variability (Ailshire and Brown 2021).
4.1. Strengths, Limitations, and Recommendations
To the best of our knowledge, this is the first report in this regard from the United Arab Emirates that provides valuable insights into their practices and gaps. A large sample size adds to the reliability of the findings. However, the study has limitations, including its reliance on self-reported data, being a single site, which may introduce bias, and its cross-sectional design, which limits the ability to establish causality. The sample consisted solely of health professional students from one university in the UAE, which may not fully represent the general population or students from other disciplines. The exclusion of other potential influencing factors, such as socioeconomic status and residential conditions, may have narrowed the scope of the findings. This study assessed self-reported behaviors rather than actual indoor air pollutant levels, which limits its ability to determine the true impact of these practices on air quality.
Despite its significance, indoor air pollution remains an under-researched area compared with outdoor air pollution. Future research should explore longitudinal studies that examine how self-care behaviors and indoor air quality impact health outcomes. Additionally, experimental studies evaluating the effectiveness of targeted educational interventions and policies to improve self-care behaviors could provide actionable insights for the curriculum and policy development. Future research should also examine the socioeconomic and environmental factors influencing IAP mitigation practices to inform targeted interventions at both the policy and individual levels.
4.2. Implications for Education, Practice, and Policy
The findings of this study highlight the need for existing national and local policies for indoor quality promotion. Despite the guidelines on indoor air quality standards, the guidelines suggest that compliance and awareness among individuals are not satisfactory. Although existing policies address indoor air pollution mitigation, gaps remain in enforcement, public awareness, and integration into daily practices. There is a need for policy optimization using data-driven decision-making methods such as TOPSIS and Taguchi techniques to prioritize and refine mitigation strategies based on their impact and feasibility. (Gajević et al. 2024). Strengthening policy enforcement mechanisms, enhancing public engagement and awareness, and incorporating indoor air quality education into academic curricula could enhance the effectiveness of current regulations and integrate these activities into daily practices. Additionally, regulatory measures, such as air quality monitoring, indoor smoking bans, and cleaner energy sources, could help establish a sustainable framework for better indoor air quality across communities.
At the individual level, students demonstrated moderate to high engagement in IAP mitigation, although gaps in behaviors suggest the low perceived importance of certain practices. The findings suggest the role of awareness campaigns and behavioral nudges based on demographics in enhancing adherence to preventive measures. Students, particularly as future leaders of environmental health, should be encouraged to model best practices for their households’ influence on the community and society at large.
CONCLUSION
Indoor air pollution is an environmental issue that can cause a range of short-term and long-term health consequences. The study found that while health professional students generally exhibited moderate to high levels of self-care behaviors related to indoor air pollution mitigation, there were notable gaps in specific practices. Gender and marital status were significantly associated with self-care practices, emphasizing the need for targeted educational intervention. The findings highlight the importance of integrating environmental health education into professional health curricula to enhance awareness and sensitivity, thereby encouraging sustainable practices. Curricular and co-curricular activities, including structured educational campaigns, workshops, and policy initiatives, can play a crucial role in improving indoor air quality practices among healthcare professionals. Addressing these gaps will not only benefit students' health but also equip them to advocate healthier living environments in their professional and personal lives.
AUTHORS’ CONTRIBUTIONS
R.K.R.: Study conception and design; V.E., P.M., S.P.P.: Data collection; A.J.: Draft manuscript.
LIST OF ABBREVIATIONS
| WHO | = World Health Organization |
| SOx | = Sulfur oxides |
| NOx | = Nitrogen oxides |
| CO | = Carbon monoxide |
| VOCs | = Volatile organic compounds |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The clearance for the study was obtained from the institutional review board of RAK Medical and Health Sciences University (RAKMHSU-REC-006-2022/23-F-N), UAE.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all the students after explaining the nature and aim of the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study are available from the corresponding author [R.K.R] upon reasonable request.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Research Ethical Committee and administrators of the college. We would like to thank all the participants of the student community for providing valuable information.


