All published articles of this journal are available on ScienceDirect.
Population Exposure to Particulate Matter and COVID-19: An Ecological Study for Health Promotion
Abstract
Background:
Documentation of the association between ambient pollution and severe coronavirus disease 2019 (COVID-19) infections are complicated and vague.
Objective:
This short research investigated the distribution of COVID-19 and its association with particulate matter before mass vaccination.
Methods:
We used the reported cases and deaths per capita and PM2.5 (particulate matter ≤ 2.5 μm) in 245 cities in the United Kingdom (UK) and United State, of America (USA) based on publicity available secondary data. We performed correlation and regression analysis between variables to explore the association between COVID-19 and PM2.5.
Results:
The analysis revealed that PM2.5 positively correlated with cases (Unstandardized Coefficient (b):150.04, P=0.006) and deaths per capita (b: 3.87, P=0.005) in total cities, after adjusting for median age and population density.
Conclusion:
The findings showed that the distribution of the disease may be affected by the PM2.5 concentration.
1. INTRODUCTION
Coronavirus 2019 or COVID-19 is the largest pandemic of the century caused by the SARS-Cov-2 virus, a new strain of the coronavirus family (Huang et al., 2020). This pandemic emerged in late 2019 and has potentially affected all health, social, economic, and environmental sectors of communities (Sarkodie and Owusu, 2020). COVID-19 is a complex, inconclusive, and contagious disease, and various factors including environmental and genetic factors are affected by the spread of its incidence and mortality (Sarmadi et al., 2020a, Sarmadi et al., 2021a, Sarmadi et al., 2021b, Sarmadi et al., 2021c). In general, environmental factors can be more than 90% effective in causing diseases (Sonnenschein and Soto, 2008). The role of environmental factors in the spread of COVID-19 is essential for communities and controlling these factors can help control and prevent the disease (Qu et al., 2020, Hadei et al., 2021). For example, due to the effect of temperature on the persistence of the virus at different levels, precise guidelines can be defined for the community. Recently, a potential link has been identified between different indicators of air pollution and COVID-19 disease (Coccia, 2021). Among air pollutants, one of the important fields of research that has had conflicting results in different parts of the world is particulate matters (PMs) (Maleki et al., 2021, Wannaz et al., 2021). PMs less than 10 microns, and especially 2.5 microns, are among the most important risk factors in various diseases (Akyuz et al., 2020, Khan, 2021), including COVID-19. Several studies have shown that there is a direct relationship between PM and the incidence of COVID-19 disease, and a number of studies have not reported this significant relationship (Cole et al., 2020, Stieb et al., 2020, Travaglio et al., 2021). A study conducted in the USA displayed a significant association between PM10 and PM2.5 and COVID-19 mortality (Wu et al., 2020). It is assumed that the SARS-Cov-2 infection causes severe lung disease caused by air pollutants, including PM2.5. In addition, other reasons for the effect of particles on the spread of the disease are the transport of the virus by PMs (Bontempi, 2020, Jayaweera et al., 2020, Setti et al., 2020b, Shao et al., 2021). Therefore, this study aimed to investigate the association between the PM2.5 concentration and the incidence and mortality caused by COVID-19 in cities in the United States and the United Kingdom.
2. METHODS
2.1. Data Collection
We gathered the total COVID-19 confirmed cases, total death, and total cases and deaths per 100,000 populations of 145 cities in the USA (from the Centers for Disease Control and Prevention (CDC) and National Health Service (NHS)) up to November 30, 2020, and 100 cities in the UK (https://coronavirus.data.gov.uk/) up to December 17, 2020, from publicly accessible databases. The data on COVID-19 were collected before mass vaccination in both counties. The data on PM2.5 were obtained from the IQAIR website (https://www.iqair.com/) for the USA and UK cities in 2019. The PM2.5 parameters were published based on the monthly mean and with microgram per cubic meters (µg/m3) unit at the Earth's surface for each city in 2020. Annual average, minimum, and maximum concentrations of PM2.5 were calculated from the monthly data measurements from each city. We included only cities that reported both the PM2.5 and COVID-19 variables.
2.2. Statistical Analysis
Descriptive analyses were performed and a bivariate correlation analysis was conducted to assess the association between PM2.5 and the number of cases and deaths of COVID-19 per 100,000 population. Furthermore, a linear regression analysis was used to estimate the association of COVID-19 cases and death ratios with a unit increase in the mean PM2.5 concentrations. It is adjusted for age>65 and population density (KM/m2) in the main model for UK cities. All statistical analyses were 2-tailed and performed at a 5% significance level using the SPSS 16 and Prism version 6 (GraphPad). It should be noted that there are differences in control policies between provinces in each country, which could impact the number and prognosis of COVID-19 patients, especially in deaths, and potentially affect the relationship between COVID-19 variables and environmental factors such as PM2.5.
3. RESULTS
As of the conducted studies in the USA and UK, a total of 5,106,109 (104,559) and 908,449 (27,614) COVID-19 cases (deaths) have been reported in 145 and 100 study cities, respectively. California, New York, and Los Angeles reported the highest number of cases and deaths in the USA and Lancashire, Kent, and Birmingham in the UK.
| Variables | Mean | SD | Median | IQR | |
|---|---|---|---|---|---|
| USA | |||||
| PCI | 3960.79 | 2051.24 | 3619.00 | 2463.00 | 4974.50 |
| PD | 64.47 | 45.40 | 53.00 | 30.00 | 86.00 |
| Mean PM2.5 | 8.51 | 2.23 | 8.50 | 7.00 | 9.90 |
| UK | |||||
| PCI | 2823.41 | 1375.81 | 2583.90 | 1653.60 | 3888.20 |
| PD | 94.48 | 37.45 | 91.95 | 64.35 | 122.60 |
| Mean PM2.5 | 9.43 | 2.17 | 9.70 | 7.38 | 11.08 |
The cases (deaths) per 100,000 population in Lubbock (Jacksonville) and Manchester (Blackpool) were much higher compared with the other states (10,380 (194) and (6,116 (189)), respectively. The mean (standard deviation: SD) of PM2.5 for the USA and UK cities were 9.43±2.17 and 8.51±2.23 µg/m3, respectively (Table 1).
| Variables | Total cases | PCI | Total deaths | PD |
|---|---|---|---|---|
| USA | ||||
| Mean PM2.5 | .260** | .137* | .294** | .305** |
| Min PM2.5 | .291** | .236** | .354** | .460** |
| Max PM2.5 | .172* | -.030 | .143 | .014 |
| UK | ||||
| Mean PM2.5 | .388** | .315** | .311** | .171 |
| Min PM2.5 | .308** | .338** | .254** | .074 |
| Max PM2.5 | .330** | .141 | .240* | .202 |
Table 2 shows the association of COVID-19 variables (absolute number and ratio) and PM2.5 contributing to the inter-city COVID-19 distribution. The association between minimum PM2.5 and COVID-19 cases and deaths was statistically significant (r=0.26 for cases and r=0.29 for deaths; P < 0.01).
After adjustment for age>65 and population density, COVID-19 cases per 100,000 population were positively associated with PM2.5 (b (SE) =157.77 (61.75), p=0.012) during the epidemic period in the UK and overall (b (SE) =150.04 (53.88), p=0.006), but it is not significant for USA cities Table 3.
| - | Unstandardized Coefficients | Standardized Coefficients | |||
|---|---|---|---|---|---|
| B | Std. Error | Beta | t | P | |
| PCI | |||||
| USA | 121.977 | 73.767 | .133 | 1.657 | .100 |
| UK | 157.767 | 61.751 | .240 | 2.555 | .012 |
| Overall | 150.036 | 53.877 | .175 | 2.785 | .006 |
| PD | |||||
| USA | 4.019 | 1.757 | .194 | 2.287 | .024 |
| UK | 2.564 | 2.223 | .142 | 1.153 | .252 |
| Overall | 3.874 | 1.373 | .187 | 2.821 | .005 |
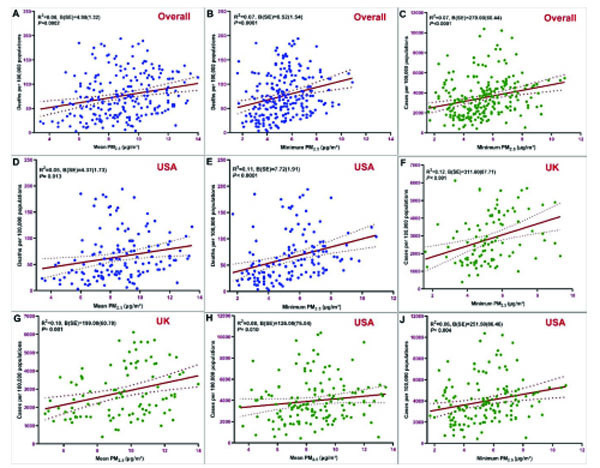
There was a positive statistically significant association between the mean PM2.5 and COVID-19 deaths per 100,000 overall (Table 3). Fig. (1) shows the standardized coefficients of the linear regression model between COVID-19 and PM2.5 parameters.
4. DISCUSSION
The results of our study showed that there is a significant correlation between PM2.5 and cases per 100,000 population (PCI) of COVID-19 disease in US and UK cities. These results are consistent with previous studies on other infectious diseases, including SARS. A study in China (2003) found that as the air pollution index (PM10 is one of the main parameters of the index) decreased from high to low, the risk of death due to SARS doubled (Cui et al., 2003). Numerous studies have confirmed the destructive effects of PM10 and PM2.5 on the lungs of individuals. The effects of particulate matter (PMs) on infectious diseases have also shown that PM2.5 can greatly increase the risk of these diseases (Domingo and Rovira, 2020, Borisova and Komisarenko, 2021). Several studies in 2020 examined the effects of air pollution on the incidence and mortality of COVID-19 in the United States (Wu et al., 2020, Sarmadi et al., 2020b, Mendy et al., 2021), the United Kingdom (Travaglio et al., 2021), China (Zhu et al., 2020, Wang et al., 2020, Yao et al., 2020), Italy (Setti et al., 2020a, Bianconi et al., 2020, Accarino et al., 2021, Borro et al., 2020, Fiasca et al., 2020, Zoran et al., 2020), Canada (Stieb et al., 2020), Netherlands (Cole et al., 2020), Japan (Azuma et al., 2020) and other parts of the world (Maleki et al., 2021). Cross-sectional studies in China have shown that high PM concentrations are significantly associated with increased incidence of disease and mortality caused by that; so the increase of every 10 micrograms per cubic meter (μg/m3) of PM2.5 concentration was associated with an increase of 0.24% in mortality (11) and 2.24% in the number of disease cases (Zhu et al., 2020). Also, increasing every 10 μg/m3 of PMs concentration was positively associated with an increased risk of positive cases of COVID-19 disease (1.05, 95% CIs: 1.04-1.07) (Wang et al., 2020). In several studies, it has been shown that long-term concentrations of pollutants are also associated with increased disease incidence (Yao et al., 2020, Stieb et al., 2020, Coccia, 2020). In a study conducted on 730 regions in 63 countries, it was found that every 10 μg/m3 increase in PM10 and PM2.5 concentrations were associated with an 8.1% and 11.5% increase in the number of COVID-19 cases (Solimini et al., 2021). A review of studies has shown that high PM concentrations are significantly associated with increased COVID-19 Morbidity and Mortality (Curtis, 2021). In a comprehensive ecological study in the United States (Wu et al., 2020), the results showed that with a unit increase in the PM2.5 concentration, the mortality rate of COVID-19 disease increased by 8% (95%: CI 2%-15%). Although the confounder variable of population density was not used in adjusting the effect of variables in this study, the results were consistent with our results. In addition, a study conducted on 355 relatively small cities in the Netherlands showed that with one unit increase in the PM2.5 concentration, the number of COVID-19 cases, hospital admissions, and deaths increased by 9.4, 3, and 2.3 units, respectively (Cole et al., 2020). Conversely, in some studies, no significant relationship was observed between PM2.5 and COVID-19 (Azuma et al., 2020).
On the other hand, our results showed that there is a positive significant correlation between the death ratio (PCD) and PM2.5 concentration in overall and USA cities; after adjusting the data for age over 65 years and population density. Although, this association was not found among the UK cities. One of the reasons for the weak correlation between the variable of death due to COVID-19 and the environmental factors can be the main interventions that are considered in connection with deaths in the hospital ward in the country. As a result, interpreting data related with the incidence of disease with PM can be more realistic and appropriate. On the other hand, it should be noted that most regions of different countries, which are at an unfavorable level in terms of air quality, maintain this situation for a long time, and as a result, people in these regions may be more susceptible to the disease (Domingo and Rovira, 2020). There are several mechanisms for the adverse effects of PM2.5 on respiratory diseases, including COVID-19. Activating inflammatory pathways in the narrow respiratory airways in response to particles may be one of the potential mechanisms (Kelly and Fussell, 2011). Another possible mechanism may be due to the effects of particles on the activities of the immune system, which affects the body's immune system (Du et al., 2016, Bashir et al., 2020). In addition, exposure to PM can increase inflammation and oxidative stress, thereby exacerbating respiratory symptoms and leading to increased hospitalizations for lung disease (Goldman et al., 2011). The virus transmission by particulate matter is another possible mechanism that has been reviewed in several studies (Alonso et al., 2015, Yang et al., 2011, Setti et al., 2020b, Bontempi, 2020, Jayaweera et al., 2020, Shao et al., 2021).
One of the advantages of the current study is the use of reliable data from small-scale companies and the evaluation of demographic confounding factors like age and population density, which are among the most significant confounding factors impacting COVID-19 illness. Moreover, the Centers for Disease Control and Prevention (CDC) and National Health Service (NHS) are two very powerful and reliable organizations in publishing COVID-19 data that belong to the United States and the United Kingdom and the data of this study have been extracted directly or indirectly from these organizations. On the other hand, the results of this study can be used for other future epidemics. The ecological studies to confirm a general hypothesis are at a lower level than individual studies but provide an overview of the association between the two variables. This study includes several limitations that should be considered in interpreting the results. A lack of access to data related to the concentration of PMs in all regions of the United Kingdom and the United States according to the IQAIR website, differences in methods of diagnosis in different countries therefore resulted in more or less reporting the numbers of patients due to different health infrastructure were factors affecting the analyses and should be considered. Ecological studies also have various inherent limitations that must be considered.
CONCLUSION
This study investigates the effect of PM2.5 on COVID-19 in the USA and the UK by adjusting confounding variables such as age and population density. In general, there is a positive and significant association between COVID-19 incidence and mortality with PM2.5 concentration. These results can be used by health decision-makers and policymakers in different parts of the community and for future epidemics.
LIST OF ABBREVIATIONS
| CDC | = Centers for Disease Control and Prevention |
| COVID-19 | = Coronavirus disease 2019 |
| NHS | = National Health Service |
| PCI | = Proportion of Cases Infected |
| PD | = Proportion of Deaths |
| PM | = Particle Matter |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome, Coronavirus 2 |
| UK | = United Kingdom |
| USA | = United States of America |
AUTHORS’ CONTRIBUTIONS
Mohammad Sarmadi: Supervision, Investigation, Data curation, Validation, Methodology, Software, Writing- Original draft preparation. Sajjad Rahimi: Conceptualization, Investigation, Data curation, Writing - Review & Editing. Maryam Feiz Arefi: Validation, Investigation, Data curation, Writing - Review & Editing. Sama Yektay: Conceptualization, Investigation, Data Curation, Writing - Review & Editing. Arash Aghabeigi: Conceptualization, Investigation, Data Curation, Writing - Review & Editing. All authors read and approved the manuscript.
ETHICAL STATEMENT
The ethics code (IR.THUMS.REC.1399.003) was obtained from the Ethics Committee of Torbat Heydariyeh University of Medical Sciences. The consent to participate is not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this article and mentioned in the Method section.
FUNDING
This work was supported by the Torbat Heydariyeh University of Medical Sciences (grant number: 99000217).
CONFLICT OF INTEREST
The authors declare they have no financial or competing interests.
ACKNOWLEDGEMENTS
The authors would like to thank the Torbat Heydariyeh University of Medical Sciences for their financial support.
REFERENCES
[CrossRef Link] [PubMed Link]
[CrossRef Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]
[CrossRef Link] [PubMed Link]


